It just so happened to be my due date when I was scheduled for induction.
Looking back, there were so many worries and challenges — and somehow, I got through each and every one of them.
- Before 12 weeks: I was afraid there would suddenly be no heartbeat.
- At 15 weeks: I worried about failing the Down syndrome screening.
- At 20 weeks: I feared that the anatomy scan might reveal abnormalities.
- Before 24 weeks: I worried that if something went wrong, I’d have to decide whether to continue the pregnancy or let go. If I lost the baby before 24 weeks, it would be treated as medical waste. Only after 24 weeks would I be allowed to collect the remains.
- At 30 weeks: I was anxious about the glucose tolerance test — if I failed, I’d have to prick my finger daily to monitor blood sugar.
- Before 30 weeks: I was afraid of preterm labor and the possibility that the baby wouldn’t survive.
- Before 34 weeks: I worried that if I went into labor early, the private hospital wouldn’t accept the case.
- At 38 weeks: I was scared of Group B Strep infection.
- Before 40 weeks: I worried about cord entanglement, reduced or excessive fetal movement, or even stillbirth.
- Before 40 weeks: I feared that if I, my husband, or my doctor contracted COVID, I wouldn’t be allowed to deliver at the private hospital.
- Before 40 weeks: I worried I wouldn’t know when to go to the hospital — that my water might break without me realizing.
- Before 40 weeks: I feared a difficult labor, and that the epidural might not work.

It happened to be my due date, and I had scheduled an induction.
Thinking back, I had so many worries and difficult moments — but amazingly, none of them actually happened. I didn’t even go into labor naturally, have a bloody show, or experience my water breaking. During my check-up, the doctor suggested inducing labor on the due date. I was able to schedule a free COVID test in advance, saving me from paying for it at the hospital.
Once the hospital booking was confirmed, I felt a lot more at ease. Even though I knew there was still a chance my water could break anytime, at least I wasn’t stuck in an endless wait.
In the few days before admission, I indulged in lots of food I hadn’t dared to eat earlier — thinking, “If anything goes wrong and I die, at least I’ll have no regrets.” I ate McDonald’s, Pizza Hut, ice cream, taro balls with grass jelly, chocolate, and more.
The day before admission, my company was attending its first-ever trade show. I couldn’t help but worry, so I went on-site to work a bit.
The night before going to the hospital, my husband helped me wash my hair extra thoroughly, since I wouldn’t be able to shower or wash my hair for a few days afterward.
On the morning of admission at 6 AM, our helper prepared breakfast for us as a send-off. The atmosphere felt a bit like heading to the airport. Around 7 AM, we hailed a taxi. Seeing how much stuff we had and that we were heading to a hospital, the driver asked, “Going to give birth?” which made me even more nervous — like I was being sent off to my doom. The whole ride was silent.
After arriving at the hospital, check-in took a long time. My urine test showed excess sugar, probably from my recent indulgence.
A nurse did an internal exam and shaved me. It was my first internal exam — her whole hand went inside, and it was very painful. I started bleeding right away. The nurse said my cervix was long and deep, and predicted a long labor.
She then asked if I intended to get an epidural. I said that unless I was already 6 cm dilated, I would definitely get it. She laughed and said that scenario is rare. The epidural costs about $6,000 HKD for the first 5 hours, and the average total is around $20,000 HKD. I did the math — I might need 15 hours of epidural.
Before inserting the induction medication, the nurse helped me empty my bowels, to avoid any embarrassment during delivery. Then she monitored the baby’s heart rate for 30 minutes. It was around 10 AM, and a friend messaged me to check in. I told her the medicine hadn’t been inserted yet, so she guessed I’d be “playing this game” till tonight.
At around 11 AM, the nurse inserted the vaginal tablet. I thought it wouldn’t hurt, but it was even more painful than the internal exam, because the nurse had to place the tablet right at the cervix and press it in. I gripped the bed pad so hard I tore it apart.
After that, my husband had to wait outside the hospital until visiting hours. I stayed in the ward to rest.
At 12 PM, I ordered delivery from the hospital canteen and enjoyed my last iced lemon tea, knowing I wouldn’t be able to have one for a while. I felt normal while eating, no discomfort or reaction — I thought to myself, “Still no signs? This is going to be a long battle.”
By 2 PM, visiting hours were over and my husband left to pass the time until the next visit.
I lay on the bed resting and chatting with friends via text. Around 3 PM, a nurse came over to chat and told me I didn’t need to stay in bed the whole time — I could walk around. I said I didn’t know where to go, and that my lower back was hurting so I didn’t want to move.
The nurse explained that the baby might be lying sideways, pressing against my spine, causing the discomfort. She suggested I try sitting on a yoga ball to help reposition the baby. I figured I had nothing better to do, so I asked her to take me.
She brought me to an empty ward, turned on the TV, taught me a few exercises using the yoga ball, and then left me to it. Some of the movements made me feel slightly uncomfortable, but nothing unbearable. At 4 PM, I left to return to the ward for my husband’s visit.
While he was with me, I started to feel something similar to period cramps, but still tolerable. I mentioned it to the nurse during her rounds, but she said based on my description, it likely wasn’t a real contraction. She explained that contractions are regular, perhaps once every 30 minutes at first, lasting several seconds each, and they would gradually become more frequent and more painful.
At 4:30 PM, the doctor came to check on me. He touched my belly and noted that the baby had moved down — a sign of progress — but said it was likely the baby wouldn’t be born until sometime before noon the next day.

Everyone kept telling me it wouldn’t happen so soon. Even the doctor and nurses — all professionals with experience — said so. During the morning check, the doctor even noted that my physical structure would make delivery more difficult than average. So I was mentally prepared for a long and painful labor. I was even thinking about when to decide on the epidural.
I used an app to track the timing of my contractions — I’d press “start” when the pain began, and “end” when it stopped. After a while, I noticed that my contractions were very regular, coming every 2 minutes and lasting about 40 seconds. Still, it was within a tolerable range. Eventually, though, the pain grew so intense I didn’t want to press the phone anymore. I asked my husband to help me track the contractions. I started wondering: Should I go ahead and request the epidural? Should I try to hold on a bit longer? Are these the “real” labor pains, or still just the early contractions?
By around 5 PM, the pain started spreading. Each time I had a contraction, I mentally debated whether I should call the nurse. But I gritted my teeth and endured each wave. And honestly, the internal exams were terrifying. I didn’t dare call the nurse unless absolutely necessary — because each check meant more pain. I remember seeing a friend’s message asking, “Did you get the epidural yet?” and that made me think, It’s probably time… After all, I chose to give birth at a private hospital just for the option of an epidural — why am I still suffering like this?
Just before 6 PM, I spoke into the intercom and told the nurse I was in a lot of pain. She came to check and did an internal exam — and surprisingly said, “You’re progressing well. You’re about 2 cm dilated — we can move you to the delivery suite!” My husband was so relieved, too — now he could stay with me full-time instead of worrying about visiting hours. He had been debating whether to go home or wait nearby overnight.
At 6 PM, the anesthesiologist was scheduled. We were told there would be a 30-minute wait. The nurse asked my husband to go enjoy a proper dinner, as they believed I wouldn’t be delivering anytime soon. I also overheard the nurse calling my OB-GYN, telling her to mentally prepare to come in, possibly around midnight.
That waiting period for the anesthesiologist was the most painful part of the whole labor. I was in such agony I just wanted to curl up into a ball — but since the fetal monitor was connected, the nurse told me I had to lie flat or the readings would go off. Worse, I had to keep my legs straight. Another nurse saw my contraction patterns on the monitor and said they were intense and frequent — spike after spike. She felt bad and offered me laughing gas, but I thought, the anesthesiologist should be arriving soon, so I declined.
Around 6:30 PM, the anesthesiologist finally arrived — still in casual clothes, not even changed into scrubs. He started explaining the risks of epidural anesthesia, but I didn’t hear a word — I just wanted him to hand me the consent form and get on with it.
Thankfully, seeing how much pain I was in, he didn’t delay. He said a few words, had me sign, and started the prep. He asked me to lie on my side in a “shrimp” position — but I was in the middle of a contraction, shivering and barely able to control my body. I felt like I was on the brink of death. Seeing this, the anesthesiologist and nurse physically dragged me into position, working together to curl me up.
Anesthesiologist: “I’m disinfecting your back now!”
Me (in my head): Please just hurry.
Anesthesiologist: “Now a small injection to numb the skin, so the real injection doesn’t hurt!”
Me: Please hurry… I sounded like an addict desperate for relief…
Anesthesiologist: “Make sure you don’t move — moving is very dangerous!”
Me: Are you kidding? Just get on with it…
Anesthesiologist: “It’s done. But the medication will take about 10 minutes to kick in.”
Me: (mentally rolling my eyes again and again)
After who knows how many more contractions, the nurse asked me to call my husband. I didn’t even know where my phone was. She handed me a phone — I almost forgot how to unlock it — and I called him. He said, “Already? I just finished dinner! You told me to take my time!” But he said he’d come right away.
At the same time, I heard the nurse calling my OB-GYN, telling her, “Please come now — she’s about to deliver.”
But I was still in pain. The anesthesiologist used an ice pack to test if the epidural had taken effect. I could feel slight coldness below the navel, but above the navel it felt really cold. He said that meant it was working — they aim to preserve about 30% of the pain sensation to allow effective pushing. But I felt like I still had 5–6 out of 10 pain, far more than I expected from “painless labor.” I didn’t say this out loud — but the anesthesiologist seemed to sense it and gave me another dose.
Then someone said, “It’s probably time to manually break the water.” I saw a glass rod with a hooked tip in front of me and thought, Is this going to hurt? I asked, “Can we wait a bit, until the epidural kicks in fully before breaking the water?” Someone answered, “Yes, we can.”

With just a blink, both the doctor and my husband had arrived. Soon after, the nurse told me, “Push now!”
I said, “Huh? Already?”
“Yes! You’re fully dilated — start pushing!”
Just a few moments ago, I had a strong urge to poop. I remembered from childbirth videos that you mustn’t push too early before full dilation, or you risk tearing. So I’d been desperately holding it in — which now felt like just minutes ago.
But suddenly, I realized I no longer felt any pain — not even the urge to poop.
And if you don’t feel like pooping… how do you know how to push?
Looking at the clock in the delivery room, it was around 7 PM. I couldn’t even tell if I was still having contractions. I just occasionally felt my belly tighten slightly — I wasn’t even sure if that was it.
“See? You can’t give birth without pain,” the nurse joked. “This is the downside of epidurals.”
But I felt amazing at that moment. Can I just take a breather first? I thought.
“Let’s reduce your epidural dosage,” she said. “You don’t know how to push otherwise.”
No no no! I thought. Just tell me when the contractions start and I’ll try to push. I don’t want to go from heaven back to that hell.
So we gave it a try.
“You’re having a contraction now. Take a deep breath, hold it for 20 seconds, and push downward with the breath. Let’s count together… 1, 2, 3 — what, you’re out of breath already? Quick, breathe again and push!”
“1, 2, 3…”
Still no luck.
“The baby’s head can’t get past the pelvis yet — let’s go again…”
And so we repeated this… maybe 100 times. The nurse said, “How about we reduce the meds? You’re not feeling anything and we’re getting nowhere.”
Alright… just a little, I agreed reluctantly.
Every time I felt a contraction, I’d try pushing. But I knew I was really just holding my breath — I wasn’t successfully pushing down. It felt nothing like trying to poop, which I had assumed it would be.
After nearly an hour, even with less anesthesia, there wasn’t much progress. The nurses began physically pushing on my belly to help move the baby down. At first, one nurse cheered me on while another pressed. Then later, two nurses — four hands — were pushing hard, forcing the baby down like I was being wrung out. I felt like a punching bag in the middle of chaos.
At this point, I had kind of given up and just let them do what they needed. Then my OB came over and calmly sat at my feet.
Suddenly, I felt a warm sensation in my vagina. I looked down and saw what looked like a half-circle shape emerging in segments, like an old-school DVD slowly ejecting from a glitchy DVD player — stuttering, inch by inch.
The doctor remained calm as always, silently catching the baby.
The nurse was yelling, “One more push! Just the body left!”
So I gave it my all, using the breathing and pushing method they taught me.
And finally… my baby was born.
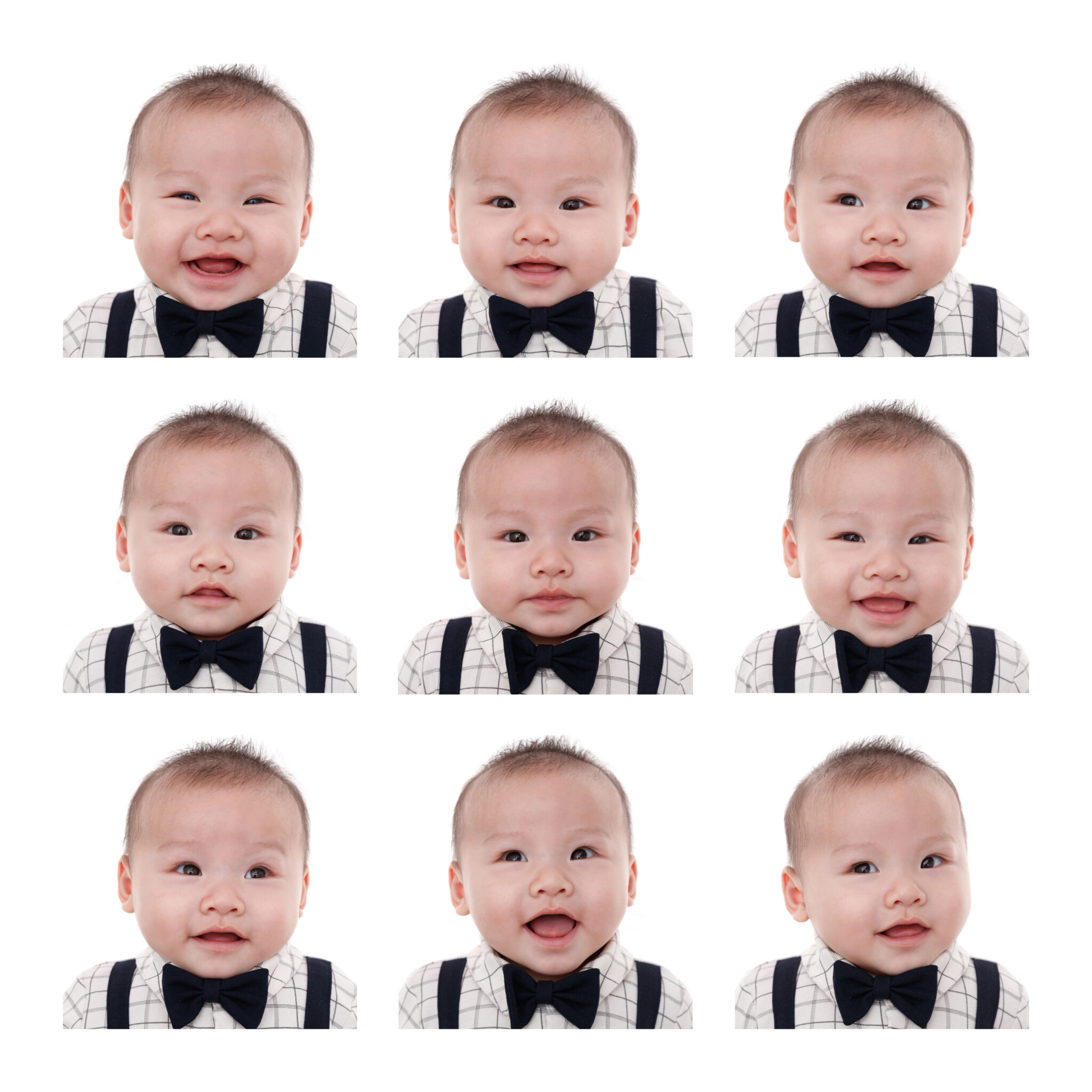
Right away, the doctor placed this bloody, slippery little body onto my belly. The baby was silent at first, and the nurse quickly used a suction tool to clear fluid from the mouth. A moment later, my baby let out a cry.
After announcing the time of birth, they handed the scissors to my husband to cut the umbilical cord, and someone took a few photos. Meanwhile, the doctor quietly delivered the placenta and began stitching me up. The nurse then took a photo of the three of us — our first family photo.
What felt like a smooth and fast birth story had finally come to a close.
Now it’s Day 3 postpartum, and I’m getting ready to leave the hospital.
I know a whole new challenge awaits once we get home.
And if I don’t write this down now, I probably won’t have the chance again.
If I still have the energy in the future, I’ll share more about parenting life with you all.